When health workers stopped visiting Ratna Jamni’s home in Pakistan to provide her with tuberculosis (TB) medication, she found herself facing an agonizing decision. With no other choice, she began making the painful journey to a clinic, moving “step by painful step, when even standing feels impossible.”
For months, the 40-year-old had been receiving care and mental health support at home as she battled drug-resistant TB. But now, those crucial visits had stopped completely.
“Every trip is painful, exhausting, and humiliating. I don’t know how much longer I can do this,” she told CNN through the Dopasi Foundation, a Pakistan-based NGO that previously provided her care through funding from the United States Agency for International Development (USAID).
“The journey is long, my body is weak, and every breath feels heavier than the last. I wonder if it’s even worth it. I wish this suffering would end – either the help returns, or I no longer have to endure this pain.”
The World’s Deadliest Infectious Disease
TB, a bacterial infection primarily affecting the lungs, remains the leading infectious cause of death worldwide. In 2023 alone, it claimed 1.25 million lives, according to the World Health Organization (WHO).
Despite its severity, TB is both preventable and treatable with the right medical interventions. Without treatment, however, it has a staggering mortality rate of nearly 50%.
Millions of TB patients, including Jamni, relied on USAID’s support for their treatment. But now, that lifeline has been severed. The Trump administration’s abrupt decision to freeze and later cut vast portions of USAID’s funding has left aid organizations scrambling—and patients suffering.
Doctors and humanitarian groups warn that these cuts could lead to thousands of preventable deaths, a surge in global TB cases, and the potential spread of an even more drug-resistant strain of the disease. Alarmingly, this crisis could also impact the United States itself.
According to a model by the UN-affiliated Stop TB Partnership, more than 11,000 additional TB patients may have died in just two months since USAID funding was largely frozen on January 24. The impact of these cuts is expected to cause global TB infections to rise by 28-32% in 2025, per an internal USAID memo from senior official Nicholas Enrich, who has since been placed on administrative leave.
A Crippling Breakdown in TB Response
Before these cuts, USAID played a crucial role in fighting TB worldwide. The agency provided grants to 24 national governments in high-TB-burden countries, as well as international and local NGOs. USAID was also deeply involved in global HIV/AIDS healthcare—an especially important factor since TB remains the leading cause of death among people living with HIV.
Dr. Lucica Ditiu, CEO of the Stop TB Partnership, described the situation as dire. Unlike previous funding adjustments, which were announced in advance, these cuts were sudden and unprecedented. “It’s very difficult for these countries overnight to find the resources” to fill the gap, she told CNN.
For the 27 hardest-hit countries, WHO reported that the funding shortfall is causing “crippling breakdowns in their TB response with devastating consequences.”
The impact varies by country, depending on how USAID funds were used. In Mozambique, for example, nearly half the country is unable to diagnose TB because the USAID-supported laboratory system is no longer functional. Many programs, such as Stop TB Partnership’s Global Drug Facility, which provides affordable TB medications, have seen partial funding restored through temporary waivers. However, in at least nine countries, access to TB drugs remains severely compromised.
The Human Toll of Funding Cuts
The hardest-hit areas are seeing severe setbacks. In Cambodia, an aid program run by local HIV and TB organization KHANA had, over the past five years, screened more than 780,000 people, traced 16,000 close contacts of TB patients, and supported 800 individuals with multi-drug-resistant TB. That program has now completely shut down.
KHANA’s executive director, Choub Sok Chamreun, painted a grim picture of the consequences. The number of new TB cases recorded in the region plummeted from 650-850 per month to just 250 in February. This drop is not due to fewer infections—it’s because people are no longer being diagnosed or receiving care.
“This means that people don’t come to services. It means that the infection continues to spread over the community … it means that the aim to end TB by 2030 is impossible,” Chamreun said, referencing the UN’s goal to largely eliminate the disease within the next five years.
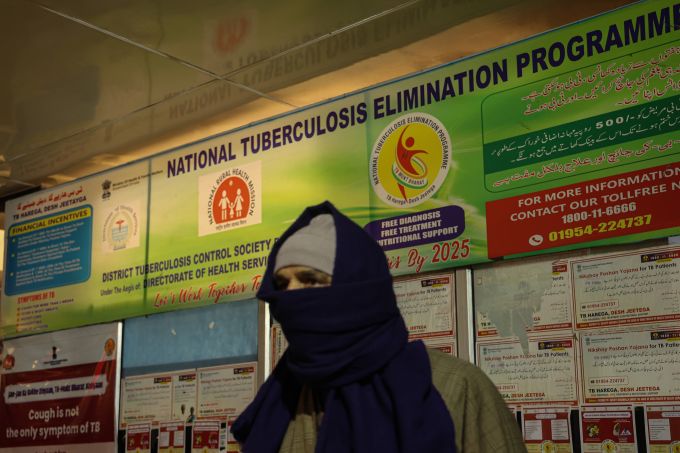
A similar crisis is unfolding in Pakistan, where USAID-supported case-finding programs in 27 districts have shut down. Without funding, the country has lost crucial tools such as transportation for sputum samples and community-based monitoring to identify barriers to TB treatment, according to Kinz ul Eman, CEO of the Dopasi Foundation.
The sudden loss of funding has also led to immediate layoffs of field health workers. “These are people who actually risked their lives to support their community,” Eman emphasized.
The Threat of Drug-Resistant TB
The impact of these funding cuts extends beyond today’s TB patients. Medical experts warn that interrupting treatment could fuel the rise of an even more dangerous, drug-resistant strain of TB. Patients who are forced to stop their four- to six-month regimen may develop a form of TB that is resistant to existing medications, making it harder to treat and easier to spread.
“Anytime you cease a treatment in the middle of the course of therapy, you promote the selection of drug resistance, and people then become contagious again to others in their community,” explained Dr. Kenneth Castro, a professor at Emory University and former director of the CDC’s TB elimination division.
With few available treatments for extreme drug-resistant TB, “you create, basically, a bug which is virtually resistant to what we have,” Ditiu warned.
This concern is not theoretical. Reports of patients being forced to ration or skip medication have already emerged. Bruce Tushabe, an official with the AIDS and Rights Alliance for Southern Africa, shared the story of a woman in Uganda who started splitting her medication with her husband. Neither of them is now receiving the full prescribed dose, putting them both at risk.
Another patient who relied on a now-closed specialist clinic is avoiding general hospitals due to the stigma surrounding TB, highlighting yet another barrier to care.
The Fallout: A Rising Global Threat
As TB rates rise worldwide, experts caution that the United States will not be immune to the consequences. Although the U.S. currently maintains one of the lowest TB rates globally—just 2.9 cases per 100,000 people—recent outbreaks signal growing concerns.
In January, Kansas City experienced a spike in TB cases, resulting in dozens of infections and at least two deaths. Meanwhile, in Europe, childhood TB cases surged by 10% in 2023, according to WHO. These warning signs indicate that TB remains an active threat.
“The irony,” Castro noted, “is that these disinvestments end up resulting in higher costs to recover and mitigate the damage done.”
As global health experts continue to sound the alarm, the question remains: Will the world act in time to prevent further devastation, or will these funding cuts mark a turning point in the battle against TB?